Gut Health and Autism

Understanding the Gut-Brain Connection in Autism
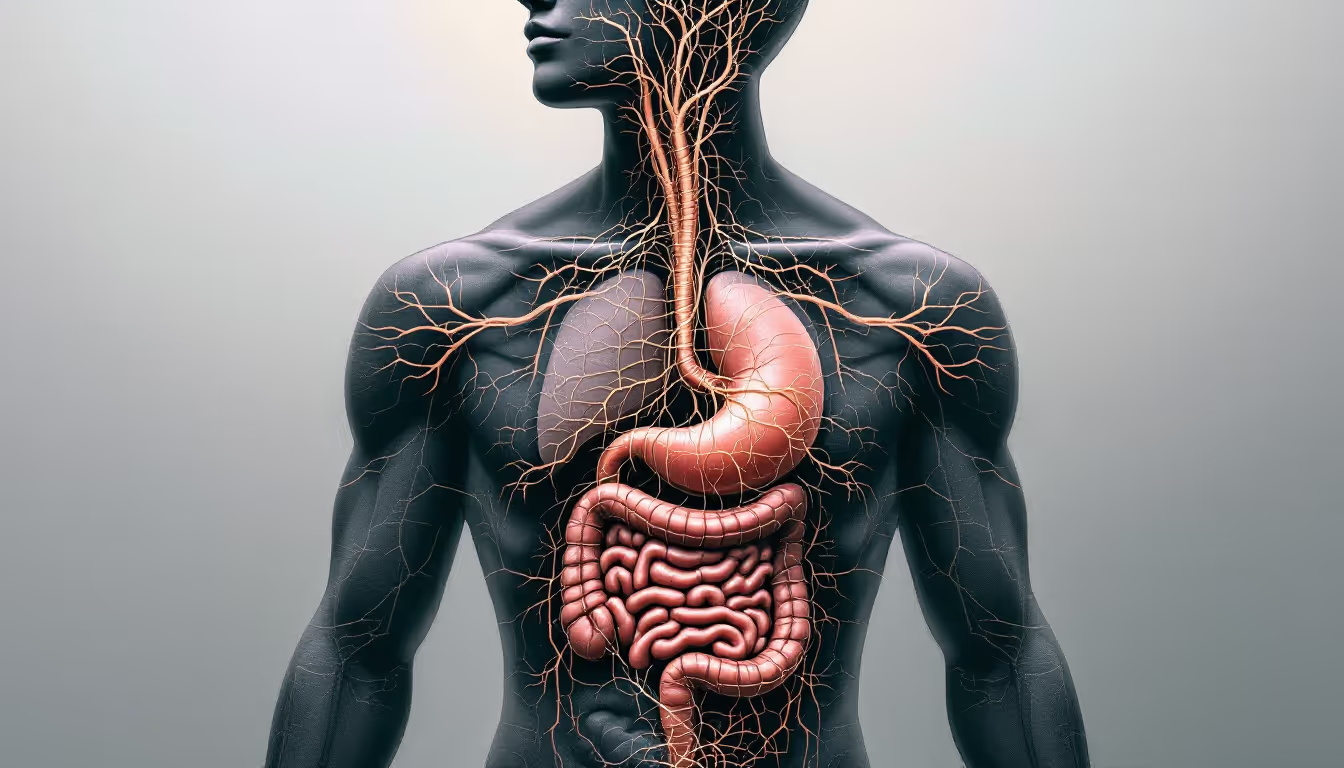
In recent years, the scientific community has increasingly explored the significant ways gut health impacts overall well-being. Among the many areas of study, the link between gut health and autism spectrum disorders (ASD) has become a particular focus. Researchers are delving into how gut microbiota — the community of microorganisms living in our digestive tracts — may influence brain development and function, potentially affecting the behavioral traits associated with autism. This exploration includes understanding gastrointestinal symptoms prevalent among autistic individuals and identifying potential therapeutic interventions that might offer relief.
The Relationship Between ASD and Gut Health

Is there a correlation between autism and gut health?
There is growing evidence of a significant correlation between Autism Spectrum Disorder (ASD) and gut health. This relationship is primarily observed through the microbiota-gut-brain axis, which indicates that gut bacteria can influence brain function and behavior. Numerous studies have highlighted that alterations in gut microbiota, or dysbiosis, may be implicated in the pathogenesis of ASD. This dysbiosis often manifests as gastrointestinal symptoms, including constipation and diarrhea, which are prevalent in many individuals with autism.
Factors such as mode of delivery, early colonization, and antibiotic use during infancy play pivotal roles in shaping gut microbiome development and potentially influencing the onset of autism. For instance, infants born via C-section have been shown to have a higher risk of developing ASD compared to those born vaginally. Additionally, early antibiotic treatments can disrupt gut flora, further increasing the risk for neurodevelopmental disorders.
Therapeutic interventions, particularly fecal microbiota transplantation (FMT) and the use of probiotics, have demonstrated promise in restoring gut balance. These approaches not only aim to improve gastrointestinal health but also show potential in alleviating core symptoms related to autism. Overall, enhancing our understanding of the gut microbiota's impact could pave the way for effective treatments addressing both digestive and neurological aspects of autism.
Gastrointestinal Issues and Autistic Individuals

What is the link between autism and gastrointestinal issues?
Gastrointestinal (GI) disorders are highly prevalent among individuals with autism spectrum disorders (ASD). Research indicates that 30-70% of autistic individuals experience these issues, significantly higher than in neurotypical peers. Common GI symptoms such as constipation, diarrhea, and abdominal pain are often noted, and these physical discomforts can exacerbate the severity of autism symptoms.
Untreated GI distress can lead to a variety of complications, including sleep disturbances, increased behavioral issues, and heightened anxiety. These problems can ultimately interfere with the overall well-being and quality of life for autistic individuals. Moreover, many children on the autism spectrum face feeding difficulties, including food selectivity and refusal, which can further complicate their nutritional needs and health.
Impact of GI issues on behavior and well-being
The presence of GI symptoms has been linked to behavioral challenges in children with autism. For instance, GI distress can manifest as irritability and aggression, further straining family dynamics and social interactions. Additionally, children with autism may struggle to communicate their GI discomfort, making diagnosis and management of these issues more complicated. As a result, addressing GI health is crucial not only for physical well-being but also for improving emotional and behavioral outcomes in children with ASD.
Maternal health factors affecting GI dysfunction and ASD
Maternal health plays a significant role in the likelihood of GI dysfunction in children with autism. Factors such as maternal obesity, diet, and stress during pregnancy can influence the developing child's gut microbiome and immune response. For instance, research suggests that infections during pregnancy may affect both gut health and neurological development in the fetus, potentially increasing the risk for autism and related GI issues in offspring. This highlights the complex interaction between maternal health, gut health, and developmental outcomes in children.
The Role of Maternal Health in Autism Development

How does maternal gut health impact autism in children?
Maternal gut health is foundational in determining a child's risk of developing autism spectrum disorder (ASD). Research shows significant differences in the gut microbiota of children with ASD compared to typically developing peers. These differences can stem from the mother's gut microbiome during pregnancy, which has crucial implications for the child's brain and immune system development.
Infections during pregnancy can lead to inflammatory responses, specifically the release of interleukin-17a (IL-17a). Increased levels of IL-17a have been associated with impaired brain development and altered immune responses in the fetus, heightening the risk for neurodevelopmental disorders, including autism.
Potential preventive interventions
Interventions targeting maternal gut health may provide possible preventive strategies against ASD. Modifying the maternal gut microbiome through dietary changes or the use of probiotics could foster a healthier environment for fetal development. Encouraging a balanced microbiome may lead to healthier immune responses and brain development for the child, potentially reducing the risk of autism.
Overall, supporting maternal gut health both prior to and during pregnancy is vital for optimizing outcomes for children and mitigating the risks associated with autism spectrum disorder.
Debunking Myths: The Complex Case of 'Leaky Gut' and Autism
Understanding 'leaky gut' and its proposed connection to ASD
Increased intestinal barrier permeability, commonly known as 'leaky gut', has gained attention in discussions about autism spectrum disorders (ASD). The theory posits that a compromised gut barrier could allow toxins and irritants from the gut to enter the bloodstream, potentially affecting brain function and behavior. Some research on rodent models has shown that disruptions to the intestinal barrier lead to negative social behaviors, while interventions aiming to repair this barrier may improve those behaviors.
Evidence supporting or refuting a direct link
Despite the intriguing findings regarding gut health, the causality between leaky gut and autism remains ambiguous. While some individuals with autism exhibit increased intestinal permeability, research indicates that these changes may arise from dietary restrictions or sensitivities, rather than being a cause of ASD itself. Additionally, various studies exploring the gut-brain axis—where gut health is linked to neurological conditions—suggest that inflammatory pathways involving lipopolysaccharides (LPS) and Toll-Like Receptor 4 (TLR4) may play a role in how gut disruptions might influence autism symptoms. Moreover, while the use of probiotics and dietary changes has potential, the controversial GAPS diet targeting ‘leaky gut’ lacks robust clinical validation.
Importance of gut-brain axis
The gut-brain axis symbolizes the intricate connection between gastrointestinal and neurological health. Disturbances in gut microbiota, observed frequently in autistic individuals, underscore the potential influence of gut health on behavior. Addressing this connection through dietary modifications or microbial therapies could pave the way for novel approaches; however, more rigorous research is necessary to clarify these relationships and to understand the underlying mechanisms at play.
Improving Gut Health in Autism: Potential Strategies

How can gut health be improved for individuals with autism?
Gut health for individuals with autism can be improved through several interventions targeting gut microbiota.
Probiotic and Prebiotic Interventions
Probiotics, particularly specific strains like Lactobacillus plantarum and Bifidobacterium, may enhance neurological function and alleviate behavioral symptoms associated with Autism Spectrum Disorder (ASD). Prebiotics also support the growth of beneficial gut bacteria.Microbiota Transfer Therapy (MTT)
This promising method involves transferring healthy gut bacteria from a donor to individuals with autism. MTT has shown beneficial effects in rebalancing gut microbiota, leading to improvements in both gastrointestinal and autism-related behavioral symptoms.Dietary Changes
Dietary interventions such as ketogenic diets and gluten-free, casein-free (GFCF) diets have been explored. While some individuals report positive responses, the effectiveness can vary significantly among individuals due to differing dietary restrictions and preferences.
A tailored approach that considers the specific needs of individuals with ASD is essential for effective improvement in gut health and overall quality of life.
| Intervention Strategy | Description | Evidence of Effectiveness |
|---|---|---|
| Probiotics | Enhances beneficial gut bacteria, relieving symptoms. | Promising but needs more research. |
| Microbiota Transfer Therapy | Transfers healthy bacteria to rebalance gut flora. | Shows significant improvements in gut health and behavior. |
| Dietary Changes | Modifications like GFCF or ketogenic diets. | Mixed results and individualized response. |
Implementing these strategies holistically can provide individuals with autism relief from gastrointestinal symptoms and potential improvements in behavioral health.
Emerging Research on Gut Microbiota and ASD

Latest Studies on Gut Microbiota Composition in ASD
Recent studies have demonstrated significant differences in gut microbiota between children with Autism Spectrum Disorder (ASD) and neurotypical children. For instance, alterations in bacterial populations were noted in children who developed autism, particularly highlighting lower diversity in gut bacteria. A study involving stool samples from over 1,600 children revealed specific microbial differences that could enhance diagnostic accuracy for autism, achieving an accuracy rate of approximately 81.6% using 31 different microbial taxa.
Role of Specific Gut Bacteria in Influencing Behavior
Dysbiosis, or an imbalance in gut microbiota, has been found in many children with ASD, which may correlate with behavioral issues. Certain beneficial bacteria, such as Bifidobacterium, have a positive impact on mood and behavior due to their role in serotonin production. Conversely, increased levels of potentially harmful bacteria like Clostridia have been associated with gastrointestinal problems and behavioral symptoms, suggesting an influential relationship between gut health and autism-related behaviors.
Long-Term Potential of Microbiota-Targeted Treatments
Therapeutic interventions aimed at restoring gut microbiome health, such as probiotics and fecal microbiota transplantation (FMT), have shown promising results. Research indicates that these interventions can lead to improvements not only in gastrointestinal symptoms but also in core ASD-related behaviors. Studies highlighted that such therapies may result in an 80% reduction in GI symptoms and a 24% improvement in autism symptoms, emphasizing the potential long-term benefits of targeting gut health in managing ASD.
Reflections on Gut Health and Autism Advocacy
Educational and Advocacy Efforts to Inform About Gut Health in Autism
Increasing awareness of the strong connection between gut health and autism spectrum disorder (ASD) is critical. Advocacy groups and educational initiatives are working diligently to inform parents, caregivers, and healthcare professionals about the significance of gastrointestinal health for autistic individuals. Understanding this relationship can facilitate timely interventions that may lead to improved health outcomes.
Challenges in Public Understanding and Scientific Communication
Despite ongoing research, the public perception of gut health and autism often remains mixed. Many misconceptions linger, particularly regarding the interpretation of scientific findings. For example, while some studies indicate that certain gut bacteria profiles are prevalent in autistic individuals, it is essential to clarify that this does not imply causation. This complexity requires clear, effective communication to help families navigating autism understand what the latest research truly signifies for their children.
Future Directions for Research and Treatment
Future research endeavors should focus on the effects of dietary interventions, gut microbiota manipulation, and specific probiotic therapies in managing ASD. As we uncover how gut health intertwines with autism, tailored treatment strategies may emerge, enhancing the quality of life for those on the spectrum. The evolving field of microbiome research promises exciting avenues for improving both gastrointestinal and neurological health in autistic individuals.
Towards a Holistic Understanding of Autism and Gut Health
The emerging narrative around gut health and autism is one of complexity and hope. While the gut microbiome's full impact on autism spectrum disorders remains to be fully understood, ongoing research provides promising insights. By piecing together how gut health affects neurological development, gastrointestinal well-being, and potentially even behavioral outcomes, scientific advancements point towards more comprehensive therapeutic strategies. Personalized treatments that leverage our growing knowledge of the microbiota-gut-brain axis could ultimately improve both the physiological and emotional lives of those on the autism spectrum. As research progresses, so will our understanding of these intricate connections, paving the way for informed interventions and a greater appreciation for the role of gut health in holistic autism care.
References
- Gut-Brain Connection in Autism | Harvard Medical School
- Role of Gut Microbiome in Autism Spectrum Disorder and Its ...
- Nutrition and the Gut-Brain Connection - Autism Research Institute
- Scientists discover gut microbiome differences in children with autism
- Spotlight on the Gut Bacteria-Brain Connection in Autism
- Autism Spectrum Disorder as a Brain‑Gut‑Microbiome Axis Disorder
- 'Strong association' between gut microbiome and autism, study finds
- Do gut microbes have a role in autism itself? - The Guardian
- The Gut, Autism, and Mental Health
- Learn Why It's Important to Understand Gut Bacteria with Autism
Recent articles

Expressive Speech Delay 2-Year-Old
Understanding and Addressing Expressive Speech Delay in Toddlers

How Speech Recognition Works
Unlocking the Power of Speech Recognition in Therapy and Healthcare

Autism and Head Size
Understanding the Complex Relationship Between Autism and Head Size

Occupational Therapy in Autism
Enhancing Independence and Quality of Life Through Occupational Therapy in Autism

Do Autistic People Understand Sarcasm?
Navigating the Nuances: Understanding Sarcasm and Social Communication in Autism

Autism Routines
Crafting Effective Daily Structures for Children with Autism


